How Ultraprocessed Foods Hijack Your Brain and Create Addiction

For decades, the idea that food could be addictive seemed far-fetched to many scientists. But mounting evidence now reveals a disturbing truth: ultraprocessed foods may be rewiring our brains in ways strikingly similar to drugs and alcohol. What began as a controversial hypothesis has evolved into a compelling body of research that's forcing us to rethink our relationship with the foods that dominate modern diets.
From Skepticism to Scientific Consensus
The journey toward understanding food addiction began with an unlikely conversation. In 2007, food policy expert Kelly Brownell, then at Yale University, and addiction researcher Mark Gold, then at the University of Florida, organized a groundbreaking two-day meeting that brought together scientists from two fields that had never seriously engaged with each other: nutrition and addiction.
The initial skepticism was palpable. "The people from the addiction field were much quicker to embrace the concept that food could be triggering addictive processes than the people in the nutrition field," Brownell recalls. The resistance made sense—nutrition scientists weren't accustomed to thinking about their research through the lens of addiction. But as evidence accumulated over the following years, the scientific community began to take the concept seriously.
Early pioneering work by neuroscientist Nicole Avena in the 2000s demonstrated that sugar consumption shared characteristics consistent with addiction, based on criteria from the Diagnostic and Statistical Manual of Mental Disorders (DSM), psychiatry's authoritative handbook for diagnosing mental health conditions. Though the idea faced resistance initially, the research momentum proved unstoppable.
Your Brain on Ultraprocessed Foods
The most compelling evidence for food addiction comes from neuroscience laboratories, where researchers have documented how ultraprocessed foods fundamentally alter brain function. The changes occur in the brain's reward regions, particularly the striatum—a deep, well-connected brain structure that influences motivation and generates feelings of pleasure.
The striatum evolved to signal when something benefits the body. For our ancestors, discovering calorie-dense foods like honey would trigger a powerful reward response, encouraging them to remember and seek out these valuable resources. This ancient system, however, never encountered the engineered foods that now fill grocery store shelves.
"When we look in the brain, there are neurochemical changes that happen in response to food that are very much like what you would see in response to drugs or alcohol," Avena explains. Scientists have identified alterations in multiple chemical messenger systems, including dopamine, serotonin, and the brain's own opioid molecules. These changes appear designed to make people hyper-alert to food cues and more motivated to eat.
Research by neuroscientist Alex DiFeliceantonio at Virginia Tech provides striking evidence of how quickly ultraprocessed foods can rewire the brain. In one study, volunteers who consumed a high-fat, high-sugar yogurt dessert daily for just two months showed stronger neural reactions to food cues in reward-related brain areas. The dessert had essentially reprogrammed their reward circuitry, amplifying their motivation to consume treats. Surprisingly, these participants also performed better on learning tasks, suggesting the brain changes were both profound and wide-reaching.
Studies using neuroimaging techniques have revealed that consumption of highly palatable foods activates similar brain regions as addictive drugs. Research has shown that foods high in fat and sugar can trigger dopamine release in the nucleus accumbens, a key reward center, comparable to what occurs with cocaine or heroin use. Over time, repeated exposure may lead to tolerance, requiring greater quantities to achieve the same pleasurable effect—a hallmark of addiction.
The Clinical Reality of Food Addiction
Beyond laboratory measurements, the human experience of struggling with ultraprocessed foods mirrors classic addiction patterns. Addiction clinician Ashley Gearhardt has witnessed this firsthand in her patients. "They're saying, 'I'm addicted to this stuff, I am telling you I'm addicted … I know it's killing me. I've got diabetes, I'm going blind, and I cannot stop,'" she recounts. Yet for years, these individuals were simply told they needed more willpower.
The Yale Food Addiction Scale, a research tool designed to assess addictive-like eating behaviors, reveals the scope of the problem. Based on nearly 300 studies from 36 countries, approximately 14 percent of adults and 12 percent of children meet the criteria for food addiction—a prevalence remarkably similar to alcohol use disorder. The assessment includes questions about eating patterns, such as whether someone ate to the point of feeling physically ill or experienced intense urges to eat specific foods.
These behaviors align with the DSM criteria for substance use disorders: intense cravings, repeated failed attempts to cut back, and continued consumption despite awareness of harm. Research has demonstrated that individuals meeting criteria for food addiction show loss of control over eating, continued use despite negative consequences, and clinically significant impairment or distress—the same benchmarks used to diagnose other addictive disorders.
Who Is Most Vulnerable?
Not everyone responds to ultraprocessed foods the same way, and scientists are working to understand why some people seem more susceptible. Preliminary findings from DiFeliceantonio's lab suggest age may play a role. Young adults aged 18 to 21 consumed significantly more when eating an ultraprocessed diet compared to a minimally processed one, and notably, they ate even when they weren't hungry. Interestingly, slightly older adults aged 22 to 25 didn't show the same pattern, suggesting developmental factors may influence vulnerability to these foods.
Research indicates that genetic factors may contribute to individual susceptibility to food addiction. Studies have identified variations in genes related to dopamine signaling that may increase risk. Additionally, early life experiences, stress levels, and pre-existing mental health conditions appear to influence who develops problematic relationships with food.
The Unique Challenge of Food
Food addiction differs from other substance use disorders in one critical way: we cannot abstain from eating entirely. Unlike alcohol or drugs, food is necessary for survival, making recovery more complex. This creates a unique challenge for those struggling with ultraprocessed foods—they must learn to navigate an environment saturated with hyperpalatable, engineered products while still meeting their nutritional needs.
The food industry's role in this crisis cannot be ignored. Ultraprocessed foods are deliberately engineered to maximize palatability through specific combinations of sugar, fat, and salt—combinations rarely found in nature. These products are designed to bypass our natural satiety signals and encourage overconsumption, raising ethical questions about corporate responsibility in the addiction crisis.
A Path Forward
Understanding food addiction doesn't mean blaming individuals for their struggles. Rather, it provides a framework for developing more effective interventions and policies. If ultraprocessed foods can indeed trigger addictive processes in the brain, then solutions must go beyond individual willpower to address the food environment itself.
Some researchers advocate for policy approaches similar to those used for tobacco and alcohol, including warning labels, restrictions on marketing to children, and taxes on ultraprocessed products. Others focus on making minimally processed, nutritious foods more accessible and affordable. Clinical interventions may include cognitive-behavioral therapy adapted for food addiction, support groups, and in some cases, medication to manage cravings.
The science is clear: for a significant portion of the population, ultraprocessed foods are not simply a matter of personal choice or willpower. They represent engineered products that can hijack ancient brain reward systems, creating patterns of consumption that meet clinical criteria for addiction. Recognizing this reality is the first step toward creating a food system that nourishes rather than exploits.
References
-
Avena, N. M., Rada, P., & Hoebel, B. G. (2008). Evidence for sugar addiction: Behavioral and neurochemical effects of intermittent, excessive sugar intake. Neuroscience & Biobehavioral Reviews, 32(1), 20-39.
-
DiFeliceantonio, A. G., Coppin, G., Rigoux, L., Edwin Thanarajah, S., Dagher, A., Tittgemeyer, M., & Small, D. M. (2018). Supra-additive effects of combining fat and carbohydrate on food reward. Cell Metabolism, 28(1), 33-44.
-
Gearhardt, A. N., Corbin, W. R., & Brownell, K. D. (2009). Preliminary validation of the Yale Food Addiction Scale. Appetite, 52(2), 430-436.
-
Gearhardt, A. N., Hebebrand, J., Potenza, M. N., Sijercic, I., White, M. A., & Burrows, T. (2023). The concept of "food addiction" helps inform the understanding of overeating and obesity: YES. The American Journal of Clinical Nutrition, 117(6), 1047-1054.
-
Lennerz, B., & Lennerz, J. K. (2018). Food addiction, high-glycemic-index carbohydrates, and obesity. Clinical Chemistry, 64(1), 64-71.
-
Schulte, E. M., Avena, N. M., & Gearhardt, A. N. (2015). Which foods may be addictive? The roles of processing, fat content, and glycemic load. PLOS ONE, 10(2), e0117959.
-
Small, D. M., & DiFeliceantonio, A. G. (2019). Processed foods and food reward. Science, 363(6425), 346-347.
-
Volkow, N. D., Wang, G. J., Tomasi, D., & Baler, R. D. (2013). Obesity and addiction: Neurobiological overlaps. Obesity Reviews, 14(1), 2-18.
-
Ziauddeen, H., & Fletcher, P. C. (2013). Is food addiction a valid and useful concept? Obesity Reviews, 14(1), 19-28.
-
Potenza, M. N., Grilo, C. M., & White, M. A. (2015). Food addiction and obesity: Diagnostic considerations. Current Psychiatry Reports, 17(12), 97.
-
Schulte, E. M., Gearhardt, A. N., & Potenza, M. N. (2016). A commentary on the "eating addiction" versus "food addiction" perspectives on addictive-like food consumption. Appetite, 115, 9-15.
-
Hebebrand, J., Albayrak, Ö., Adan, R., Antel, J., Dieguez, C., de Jong, J., ... & Dickson, S. L. (2014). "Eating addiction", rather than "food addiction", better captures addictive-like eating behavior. Neuroscience & Biobehavioral Reviews, 47, 295-306.
2 comments
October 14, 2025
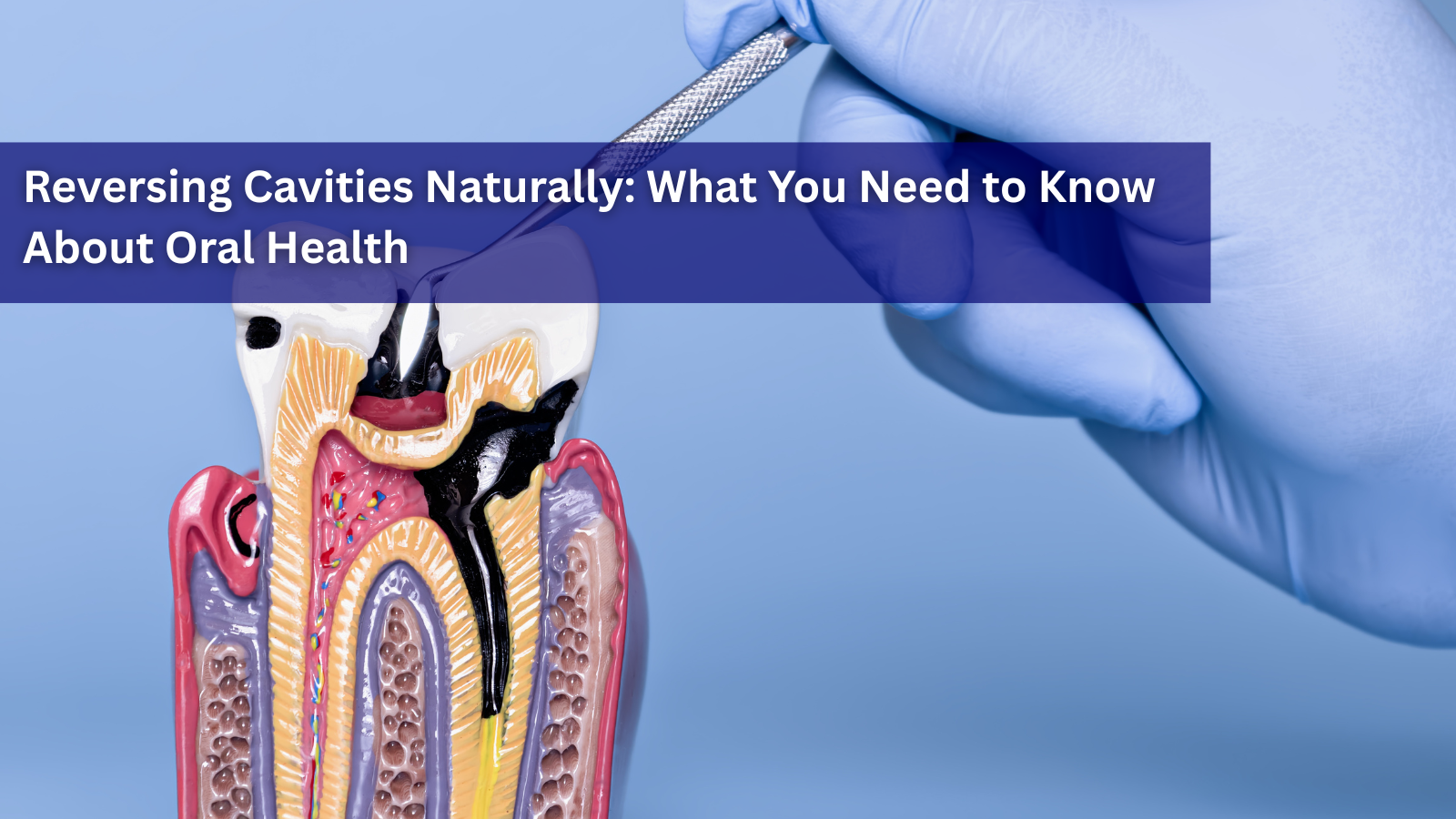
Reversing Cavities Naturally: What You Need to Know About Oral Health
It All Starts in the Mouth: Your Gateway to Health You don’t often hear about reversing cavities naturally — not because it’s impossible, but because it’s rarely discussed. Much of modern dentistry focuses on treatment rather than preven...
Read more
October 14, 2025
Some Historic Policy Shifts Against Animal Cruelty
When President Donald Trump made animal cruelty a federal crime in 2019, it marked the beginning of a sweeping transformation in how the federal government approaches animal welfare. Now, in his second term, the administration is quietl...
Read more
October 14, 2025
Who Was Michio Kushi? The Pioneer Who Exposed the Truth About "The New Human Race" and Synthetic Medicine & Food
In 1979, Michio Kushi, a prominent Japanese health food pioneer, delivered a powerful message to the world. He boldly exposed the dangers of the growing trend of synthetic medicine and foods in his work, The New Human Race. At a time wh...
Read more




Highly recommend this book on the subject of sugar addiction:
The Sugar Addiction Trap by Daybreak Mitchelson
I would love to know more about this subject.
Leave a comment