Irritable Bowel Syndrome: Understanding This Common Digestive Disorder

If you’re experiencing persistent belly pain, changes in bowel movements, and digestive discomfort that disrupts your daily life, you’re not alone. irritable bowel syndrome affects millions of people worldwide, making it one of the most common gastrointestinal disorders. Despite its prevalence, many people struggle to understand this complex condition and find effective ways to manage their symptoms.
This comprehensive guide will help you understand everything about irritable bowel syndrome IBS, from recognizing the symptoms to exploring treatment options that can significantly improve your quality of life. Whether you’re newly diagnosed or have been living with IBS symptoms for years, you’ll discover practical strategies and medical insights to better manage this functional disorder.
What Is Irritable Bowel Syndrome?
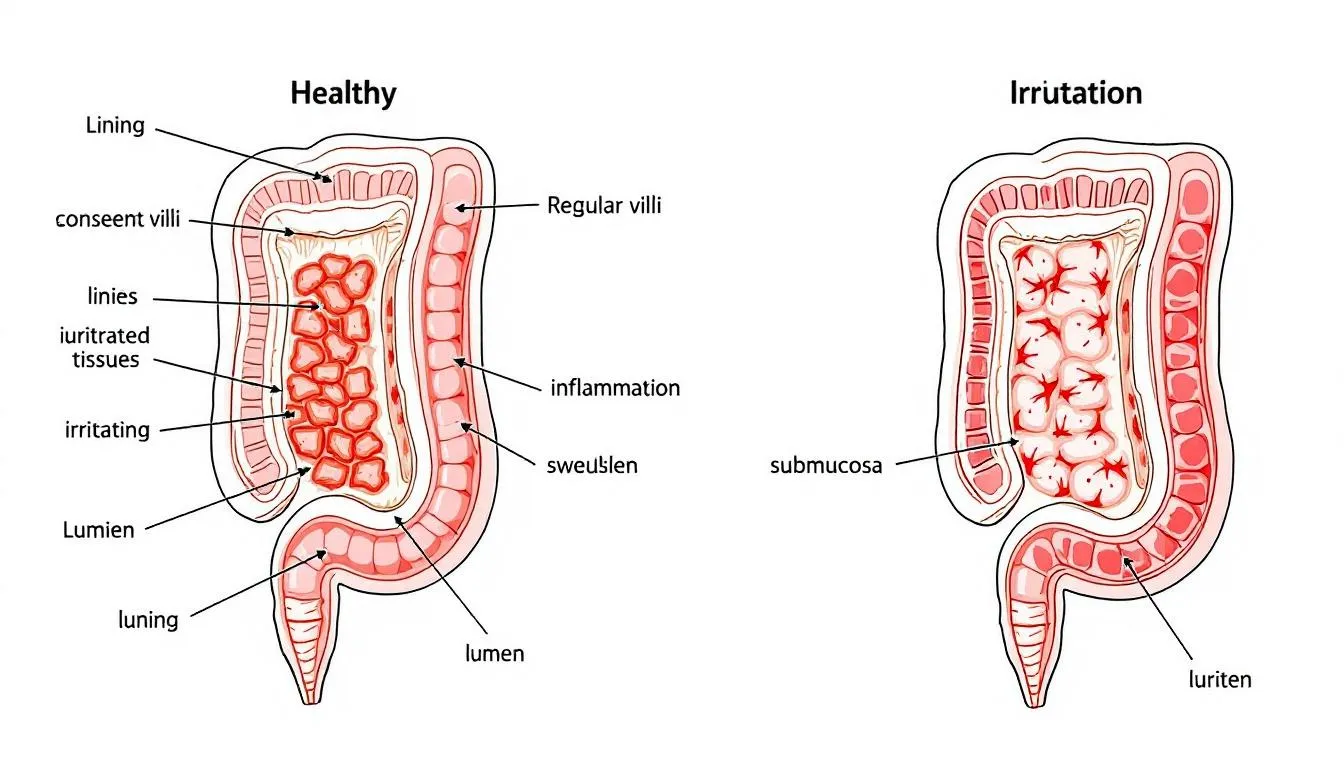
Irritable bowel syndrome is a chronic functional gastrointestinal disorder that primarily affects the large intestine, causing a constellation of uncomfortable symptoms that can significantly impact daily activities. Unlike inflammatory bowel disease or other serious diseases, IBS is classified as a functional disorder, meaning it causes real symptoms without any visible structural damage to the digestive system.

The hallmark characteristics of this bowel disorder include recurrent abdominal pain, abdominal cramping, bloating, excessive gas, and notable changes in bowel habits. These symptoms occur without any identifiable structural abnormalities in the gastrointestinal tract, distinguishing IBS from conditions like celiac disease or colon cancer.
Current statistics reveal that irritable bowel syndrome affects approximately 7-16% of U.S. adults, with women being twice as likely to develop the condition compared to men. The peak onset typically occurs between ages 20-40, though ibs occurs across all age groups. This prevalence makes IBS one of the most frequently diagnosed functional gastrointestinal disorders in clinical practice.
The distinction between functional and organic bowel diseases is crucial for understanding IBS. While inflammatory bowel disease involves visible inflammation and tissue damage that can be detected through medical imaging or biopsies, IBS presents with symptoms arising from altered gut function rather than structural abnormalities. This fundamental difference affects both diagnosis and treatment approaches.
Common Symptoms and Types of IBS
The diagnosis of irritable bowel syndrome requires specific symptom criteria, primarily recurrent abdominal pain occurring at least one day per week for the past three months. This pain typically associates with changes in stool frequency, appearance, or both, creating distinct patterns that help healthcare providers categorize the condition.
Medical professionals classify IBS into three main subtypes based on predominant bowel symptoms:
IBS-C (Constipation-Predominant): This constipation predominant ibs variant affects approximately 35% of ibs patients. Individuals experience infrequent, hard stools that require significant straining during bowel movements. Many report a persistent feeling of incomplete evacuation, even after successful bowel movement attempts. The digestive system moves waste material too slowly, leading to excessive water absorption and hard, difficult-to-pass stools.
IBS-D (Diarrhea-Predominant): diarrhea predominant ibs represents another significant category, characterized by loose, frequent stools that create urgency and increase the risk of incontinence. Patients often experience frequent diarrhea that disrupts work, social activities, and sleep patterns. The rapid transit time through the intestinal tract prevents adequate water absorption, resulting in loose, watery bowel movements.
IBS-M (Mixed Pattern): This variant involves mixed bowel habits, where individuals alternate between constipation and diarrhea episodes. The unpredictable nature of symptoms makes this particularly challenging to manage, as treatment strategies must address both ends of the spectrum.
Beyond the primary bowel symptoms, people with ibs frequently experience additional manifestations that significantly impact their quality of life. These include:
-
Visible mucus in stool, which can be alarming but typically indicates intestinal irritation rather than serious disease
-
Severe bloating that may cause visible abdominal distension
-
Excessive gas production leading to social embarrassment and discomfort
-
Persistent sensation of incomplete bowel evacuation
-
nighttime symptoms that disrupt sleep patterns
Understanding these symptom patterns helps both patients and healthcare providers develop targeted treatment strategies for effective symptom management.
What Causes Irritable Bowel Syndrome?
The exact mechanisms underlying irritable bowel syndrome remain complex and multifactorial, involving intricate interactions between the nervous system, digestive tract, and psychological factors. Research has identified several key pathways that contribute to the development and persistence of ibs symptoms.
Gut-Brain Axis Dysfunction: The communication network between the intestinal nervous system and the brain plays a crucial role in normal digestive function. In people with ibs, this bidirectional communication becomes disrupted, leading to abnormal responses to normal digestive processes. This dysfunction affects both the perception of intestinal sensations and the coordination of bowel function.
Visceral Hypersensitivity: Many ibs patients develop heightened sensitivity to normal intestinal sensations, experiencing pain or discomfort from gas, stool, or normal digestive processes that wouldn’t typically cause symptoms. This increased sensitivity helps explain why routine digestive activities can trigger significant abdominal pain in susceptible individuals.
Intestinal Motility Disorders: The digestive system relies on coordinated muscle contractions to move food and waste through the gastrointestinal tract. In IBS, these contractions may become too strong (causing diarrhea) or too weak (leading to constipation), disrupting normal bowel function and contributing to abdominal cramping.
Gut Microbiome Imbalances: Emerging research highlights the importance of intestinal bacteria in maintaining digestive health. small intestinal bacterial overgrowth and other forms of bacterial overgrowth can disrupt normal digestive processes, contributing to gas, bloating, and altered bowel movements. The delicate balance of beneficial bacteria may become disturbed, affecting immune function and intestinal inflammation.
post infectious ibs: Approximately 10-15% of IBS cases develop following a severe infection of the digestive tract, such as gastroenteritis or food poisoning. This post-infectious variant demonstrates how severe infection can trigger long-lasting changes in gut function, even after the initial infection has resolved.
Genetic Predisposition: family history plays a significant role in IBS development, with studies showing increased risk among first-degree relatives of affected individuals. While specific genetic markers haven’t been definitively identified, the clustering of cases within families suggests inherited susceptibility factors.
Common Triggers and Risk Factors
Understanding what triggers ibs symptoms is essential for effective symptom management and reducing the frequency of flare-ups. Multiple factors can precipitate or worsen symptoms, and identifying personal triggers often requires careful observation and documentation.
Dietary Triggers: certain foods consistently trigger symptoms in many ibs patients, though individual sensitivities vary significantly. High-FODMAP foods (fermentable oligosaccharides, disaccharides, monosaccharides, and polyols) frequently worsen symptoms by increasing gas production and drawing water into the intestines. Common culprits include:
-
Fatty foods that slow gastric emptying and increase sensitivity
-
Caffeine and alcohol, which can stimulate intestinal contractions
-
Artificial sweeteners that may have laxative effects
-
Dairy products in those with lactose intolerance
-
High-fiber foods that may worsen symptoms in some individuals
Stress and Emotional Factors: psychological stress represents one of the most significant triggers for IBS symptoms. The gut-brain connection means that emotional stress, anxiety, depression, and major life changes can directly affect digestive function. Many patients notice symptom flare-ups during periods of increased stress, work pressure, or emotional upheaval.
Hormonal Fluctuations: Women with IBS often experience symptom changes related to their menstrual cycle, with many reporting worsened symptoms during menstruation. These hormonal influences help explain why women develop IBS at twice the rate of men and may experience different symptom patterns throughout their reproductive years.
Medications: Certain medications can trigger or worsen ibs symptoms. Antibiotics can disrupt the normal gut microbiome, leading to temporary or prolonged digestive issues. NSAIDs may increase intestinal inflammation, while some antidepressants can affect bowel function. Patients should discuss medication effects with their healthcare providers.
Sleep Disturbances and Irregular Patterns: Poor sleep quality and irregular eating schedules can disrupt the normal circadian rhythms that govern digestive function. Maintaining consistent meal times and adequate sleep helps support optimal bowel function and may reduce symptom severity.
Age Factors: While ibs occurs across all age groups, the most common onset occurs between ages 20-40. Early adult life often involves significant stress, dietary changes, and lifestyle adjustments that may contribute to symptom development during this period.
When to See a Healthcare Provider
Recognizing when digestive symptoms warrant medical evaluation is crucial for obtaining appropriate diagnosis and treatment. While many people experience occasional digestive discomfort, certain patterns and symptoms indicate the need for professional assessment.
Persistent Symptom Patterns: If you experience abdominal pain and changes in bowel habits lasting more than three months, medical evaluation is warranted. The chronic nature of these symptoms, combined with their impact on daily activities, suggests the need for comprehensive assessment to diagnose ibs or rule out other serious diseases.
Red Flag Symptoms: Certain warning signs require immediate medical attention, as they may indicate conditions more serious than IBS:
-
rectal bleeding or blood in stool, which may suggest inflammatory bowel disease, polyps, or malignancy
-
unexplained weight loss that occurs without intentional dietary changes
-
severe nighttime symptoms that consistently disrupt sleep
-
Fever accompanying digestive symptoms
-
Progressive worsening of symptoms over time

family history Considerations: Individuals with family history of inflammatory bowel disease, celiac disease, or colorectal cancer should seek evaluation sooner rather than later. Genetic predisposition increases the risk of these conditions, making early assessment particularly important for proper differential diagnosis.
Quality of Life Impact: When bowel symptoms significantly impact work performance, social activities, or emotional well-being, professional help becomes essential. IBS can cause substantial disability if left unmanaged, but effective treatments can dramatically improve quality of life and functional capacity.
Age-Related Factors: New onset of digestive symptoms after age 45 warrants more thorough evaluation, as the risk of organic diseases increases with age. Healthcare providers typically recommend more extensive testing in older adults to ensure proper diagnosis and rule out malignancy.
Diagnosis and Medical Evaluation
Diagnosing ibs relies primarily on symptom-based criteria rather than specific diagnostic tests, as no single test can definitively confirm the condition. Healthcare providers use established guidelines and selective testing to reach an accurate diagnosis while excluding other conditions.
Rome IV Criteria: The current gold standard for ibs diagnosed involves the Rome IV criteria, which require recurrent abdominal pain averaging at least one day per week during the previous three months, along with two or more of the following characteristics:
-
Pain related to defecation (either improving or worsening)
-
Changes in stool frequency
-
Changes in stool form or appearance
These criteria help standardize diagnosis across healthcare providers and ensure consistent application of diagnostic standards.
Medical History and Physical Examination: A thorough medical history forms the foundation of IBS diagnosis. Healthcare providers assess symptom patterns, triggers, family history, and psychosocial factors. The physical examination typically reveals normal findings, though providers may note abdominal tenderness or bloating during symptomatic periods.
Limited Diagnostic Testing: Unlike many medical conditions, extensive testing isn’t routinely required to diagnose ibs. However, healthcare providers may order specific tests based on individual circumstances:
-
Complete blood count to check for anemia or signs of inflammation
-
blood tests for inflammatory markers (C-reactive protein) to screen for inflammatory bowel disease
-
celiac disease screening through specific antibody tests
-
Stool tests for calprotectin, lactoferrin, and pathogen detection when indicated
Advanced Testing Considerations: Colonoscopy isn’t routinely performed for IBS diagnosis but may be recommended for patients over 45 or those with alarm symptoms. This procedure helps rule out structural abnormalities, inflammatory bowel disease, or malignancy that could mimic IBS symptoms.
Differential Diagnosis Process: Healthcare providers must systematically rule out other conditions that can present with similar symptoms. This process involves considering inflammatory bowel disease, celiac disease, small intestinal bacterial overgrowth, lactose intolerance, and other gastrointestinal disorders. The absence of alarm symptoms and normal screening tests supports an IBS diagnosis.
The diagnostic process emphasizes the importance of building a strong patient-provider relationship, as ongoing communication helps refine the diagnosis and optimize treatment strategies over time.
Treatment and Management Strategies
Effective treatment of irritable bowel syndrome requires a comprehensive, individualized approach that addresses the multifactorial nature of this condition. Since no single treatment works for all ibs patients, healthcare providers typically combine dietary modifications, lifestyle changes, medications, and psychological therapies to achieve optimal symptom relief.
Dietary Modifications: Nutritional interventions form the cornerstone of IBS management, with several evidence-based approaches showing significant efficacy:
The low-FODMAP diet represents one of the most effective dietary strategies for many people with ibs. This approach involves eliminating high-FODMAP foods for 2-6 weeks, followed by systematic reintroduction to identify specific triggers. Research shows that approximately 70% of patients experience significant symptom improvement with this approach.
soluble fiber supplementation can benefit patients with constipation predominant ibs, helping to normalize stool consistency and improve bowel movement frequency. Sources include psyllium husk and methylcellulose, which are generally better tolerated than insoluble fiber sources that may worsen symptoms initially.
Working with a registered dietitian ensures proper implementation of dietary changes while preventing nutritional deficiencies that can occur with restrictive eating patterns.
Lifestyle Modifications: Simple lifestyle changes can significantly impact symptom severity and frequency:
-
Regular exercise improves gut motility, reduces stress, and enhances overall well-being
-
Stress management techniques, including meditation, yoga, and deep breathing exercises
-
Maintaining adequate sleep hygiene and consistent sleep schedules
-
Establishing regular meal times and eating smaller, more frequent meals

Pharmacological Treatments: Medication selection depends on the predominant symptom pattern:
For constipation predominant ibs:
-
Polyethylene glycol (MiraLAX) provides gentle, effective relief for chronic constipation
-
Lubiprostone (Amitiza) increases intestinal fluid secretion and motility
-
Linaclotide (Linzess) targets both pain and constipation through specific receptor activation
For diarrhea predominant ibs:
-
Loperamide (Imodium) slows intestinal transit and reduces stool frequency
-
Rifaximin (Xifaxan) targets bacterial overgrowth and has shown sustained benefits
-
Alosetron (Lotronex) is reserved for severe cases due to potential side effects
Antispasmodic Medications: These drugs help reduce pain and intestinal spasms:
-
Dicyclomine (Bentyl) and hyoscyamine (Levsin) provide targeted relief for abdominal cramping
-
anticholinergic medications may help reduce intestinal contractions and associated pain
Psychological Therapies: The strong gut-brain connection makes psychological interventions particularly effective:
-
Cognitive behavioral therapy helps patients develop coping strategies and address stress-related triggers
-
Gut-directed hypnotherapy has shown remarkable efficacy in clinical trials
-
Mindfulness-based stress reduction techniques can significantly improve symptoms and quality of life
Dietary Management Approaches
Implementing effective dietary strategies requires a systematic approach that balances symptom relief with nutritional adequacy. The low-FODMAP diet, while highly effective, requires careful guidance to ensure proper execution and prevent nutritional deficiencies.
Low-FODMAP Implementation: This evidence-based approach involves three distinct phases:
-
Elimination Phase (2-6 weeks): Complete removal of high-FODMAP foods to allow symptom resolution
-
Reintroduction Phase (6-8 weeks): Systematic testing of individual FODMAP groups to identify specific triggers
-
Personalization Phase (ongoing): Development of a sustainable, individualized eating plan
Fiber Management: While soluble fiber can benefit many ibs patients, implementation requires careful attention to timing and dosage. Psyllium husk and methylcellulose provide effective options that are generally well-tolerated when introduced gradually.
Probiotic Considerations: Specific bacterial strains have shown promise in clinical trials, including Bifidobacterium infantis and Lactobacillus plantarum. However, probiotic selection should be evidence-based rather than generic, as different strains provide different benefits.
Food Diary Implementation: Systematic tracking of food intake, symptoms, and triggers helps identify personal patterns that may not follow typical recommendations. This personalized approach often reveals unique sensitivities that guide individualized treatment plans.
Long-term Outlook and Complications
Understanding the long-term prognosis of irritable bowel syndrome helps patients develop realistic expectations and effective coping strategies. While IBS is a chronic condition requiring ongoing management, it’s important to emphasize that it’s not life-threatening and doesn’t increase the risk of serious complications like colon cancer.
Chronic Nature with Variable Symptoms: ibs symptoms typically fluctuate over time, with periods of relative remission alternating with symptomatic flare-ups. Many patients experience gradual improvement in symptom severity as they identify effective management strategies and develop better coping mechanisms. The condition doesn’t progress to more serious diseases or cause permanent damage to the digestive tract.
Physical Complications: While IBS itself doesn’t cause structural damage, chronic symptoms can lead to secondary complications:
-
Hemorrhoids may develop from frequent straining during bowel movements in constipation predominant patients
-
Anal fissures can occur from passing hard stools or frequent diarrhea
-
These complications are treatable and don’t represent dangerous progression of the underlying condition
Quality of Life Impact: The psychological and social effects of IBS often represent the most significant long-term challenges:
-
Increased rates of anxiety and depression compared to the general population
-
Social isolation due to unpredictable symptoms and fear of symptom flare-ups
-
Reduced participation in social activities, travel, and recreational pursuits
-
Strained relationships due to chronic symptoms and frequent medical appointments
Work and Productivity Effects: Studies consistently demonstrate that IBS significantly impacts work performance and attendance:
-
Increased sick days and medical leave compared to healthy individuals
-
Reduced productivity during symptomatic periods
-
Career limitations due to symptom unpredictability
-
Financial impact from medical costs and lost wages
Psychological Considerations: The chronic nature of IBS can contribute to mood disorders and emotional distress. However, addressing these psychological aspects through appropriate therapy often leads to significant improvement in both mental health and physical symptoms. The strong gut-brain connection means that treating depression or anxiety can directly benefit digestive symptoms.
Reassurance About Cancer Risk: One of the most important aspects of long-term outlook involves reassuring patients that IBS doesn’t increase the risk of developing colon cancer or inflammatory bowel disease. This functional disorder doesn’t cause the type of cellular damage associated with malignancy, providing important peace of mind for long-term management.
Living with IBS: Practical Tips
Successfully managing irritable bowel syndrome requires developing practical strategies that fit into daily life while minimizing symptom impact. These evidence-based approaches help patients maintain independence and improve their overall quality of life.
Establishing Eating Routines: Consistent meal timing helps regulate digestive function and reduces symptom unpredictability:
-
Eating smaller, more frequent meals reduces the burden on the digestive system
-
Maintaining regular meal times helps establish predictable bowel patterns
-
Avoiding large meals, especially in the evening, can prevent nighttime symptoms
-
Allowing adequate time for meals and avoiding rushed eating improves digestion
Stress Reduction Techniques: Since psychological stress represents a major trigger for many patients, developing effective stress management becomes essential:
-
Daily meditation or mindfulness practice, even for just 10-15 minutes
-
Regular physical activity, which provides both stress relief and improved gut motility
-
Deep breathing exercises during acute symptom episodes
-
Progressive muscle relaxation techniques for managing chronic tension

Building Healthcare Relationships: Establishing strong communication with healthcare providers ensures optimal ongoing management:
-
Regular follow-up appointments to assess treatment effectiveness
-
Open communication about symptom changes and treatment response
-
Collaborative approach to adjusting medications and dietary strategies
-
Access to mental health support when needed
The key to successful long-term management lies in developing a personalized approach that combines medical treatment with practical lifestyle strategies. While irritable bowel syndrome presents ongoing challenges, most patients can achieve significant symptom relief and maintain active, fulfilling lives through comprehensive management approaches.
Regular communication with healthcare providers, commitment to evidence-based treatments, and development of strong coping strategies form the foundation for successful long-term management. Remember that IBS is a manageable condition, and with proper support and treatment, you can significantly reduce its impact on your daily life and overall well-bein
The Most Effective Herbal Treatments for IBS
When it comes to managing irritable bowel syndrome (IBS), many patients look beyond prescription medications for relief. Herbal remedies are becoming increasingly popular because they offer natural ways to calm the digestive system, reduce inflammation, and support gut health. Among the most promising options, boswellia serrata stands out.
Boswellia Serrata (Indian Frankincense)
Boswellia, an herbal extract derived from the resin of the Boswellia serrata tree, has been used for centuries in traditional medicine to treat inflammatory conditions. Modern research suggests it may also play a powerful role in helping IBS and IBD patients achieve remission.
Boswellia works by:
- Reducing inflammation and swelling in the intestines
- Restoring normal bowel cell structures
- Improving stool consistency and properties
- Helping heal tiny openings in the bowel wall
 In fact, one clinical study published in the European Journal of Medical Research tested boswellia’s effectiveness by giving participants 350 milligrams of boswellia extract three times daily for six weeks. The results were striking: patients experienced improvements across all tested parameters, and an impressive 82% of participants with inflammatory bowel disease (IBD) went into remission. Remarkably, this was even higher than the remission rates seen with sulfasalazine, a common prescription medication for IBD.
In fact, one clinical study published in the European Journal of Medical Research tested boswellia’s effectiveness by giving participants 350 milligrams of boswellia extract three times daily for six weeks. The results were striking: patients experienced improvements across all tested parameters, and an impressive 82% of participants with inflammatory bowel disease (IBD) went into remission. Remarkably, this was even higher than the remission rates seen with sulfasalazine, a common prescription medication for IBD.
This makes boswellia a powerful herbal ally for those seeking natural IBS and IBD support.
Curcumin (Turmeric) ± Fennel Essential Oil
Why it may help: Curcumin is anti-inflammatory/antioxidant; fennel is carminative and antispasmodic, reducing gas and cramping.
Evidence: Small RCTs and pilot data suggest improved global IBS symptoms and quality of life; one double-blind trial found a curcumin + fennel essential oil combo superior to placebo over ~30 days.
Typical use: Standardized curcumin extract ~500–1000 mg/day in divided doses is common in studies; some proprietary combinations include modest curcumin plus fennel EO.
Safety notes: May interact with anticoagulants/antiplatelets; avoid with active gallstones/biliary obstruction. Can cause mild GI upset in some.
3 comments

September 27, 2025
Immune Supplements: Top 10 Best Supplements to Boost Immunity
Are you looking for effective ways to enhance your body’s natural defense? Immune supplements have become popular choices to support the immune system booster function, especially in times of increased illness risk. With so many products...
Read more
September 27, 2025
Cell Phone and WiFi Safety: How to Prevent and Treat EMF Damage and Electrosensitivity
Electrohypersensitivity (EHS), often called electrosensitivity, has been a polarizing and increasingly relevant issue over the past decade and a half. Since the number of people identifying with these symptoms continues to grow exponent...
Read more
September 27, 2025
Raw Carrots: Nature’s Antibacterial & Antiseptic Food
For most of us, carrots are simply a crunchy snack or a source of vitamin A. But according to researcher Ray Peat, PhD, raw carrots offer something more unusual: they act as a kind of natural antiseptic inside the gut, helping to contro...
Read more




I was diagnosed with Parkinson’s disease four years ago. For over two years, I relied on prescription medications and therapies, but unfortunately, the symptoms continued to worsen. My mobility declined, tremors increased, and I experienced growing fatigue and discomfort that affected my daily life. Last year, out of desperation and hope, I decided to try an herbal treatment program from NaturePath Herbal Clinic. Honestly, I was skeptical at first, but within a few months of starting the treatment, I began to notice real changes. My energy improved, the discomfort eased, and I felt stronger and more capable in my daily life. Incredibly, I also regained much of my stamina, balance, and confidence. It’s been a life-changing experience I feel more like myself again, better than I’ve felt in years. If you or a loved one is struggling with Parkinson’s disease, I truly recommend looking into their natural approach. You can visit their website at www. naturepathherbalclinic .com
I was diagnosed with Parkinson’s disease four years ago. For over two years, I relied on prescription medications and therapies, but unfortunately, the symptoms continued to worsen. My mobility declined, tremors increased, and I experienced growing fatigue and discomfort that affected my daily life. Last year, out of desperation and hope, I decided to try an herbal treatment program from NaturePath Herbal Clinic. Honestly, I was skeptical at first, but within a few months of starting the treatment, I began to notice real changes. My energy improved, the discomfort eased, and I felt stronger and more capable in my daily life. Incredibly, I also regained much of my stamina, balance, and confidence. It’s been a life-changing experience I feel more like myself again, better than I’ve felt in years. If you or a loved one is struggling with Parkinson’s disease, I truly recommend looking into their natural approach. You can visit their website at www. naturepathherbalclinic .com
This is a misleading article. The primary cause of IBS is GENETICALLY MODIFIED FOODS and CONSTANT STRESS. Whoever wrote your article is an idiot. Why post stupid propaganda that doesn’t help anyone? JUST TELL PEOPLE TO QUIT EATING GMO FOODS AND TO LOWER THEIR STRESS LEVELS AS THE #1 START TO FIXING THIS PROBLEM.
Leave a comment